When Charlotte Curtis woke up unable to see out of one eye, she learned – again – what it means to have sickle cell disease (SCD).
“You don’t know how it’s going to impact you until it does,” says Curtis, a 34-year-old mom who works in government affairs in Washington, D.C., in the US.
SCD is a lifelong condition that can damage any part of the body where blood flows. For Curtis, tiny blood vessels in her eye had started to bleed. She needed to act quickly.
Unfortunately, her eye doctor wasn’t familiar with SCD and downplayed the risks – potentially putting her in danger of losing her sight. To make matters worse, Curtis didn’t have another expert to turn to.
Not having a doctor with expertise in SCD is a common challenge for people living with the disease. In fact, in a survey completed in 2014, only 20% of family physicians surveyed in the US said they felt comfortable caring for patients with SCD.1
The disease is not new. It was first reported in 1846. In the US, it is the most common genetic disease, affecting approximately 100 000 children and adults.2 There are about 6.4 million people with SCD worldwide, more than 5 million of whom live in sub-Saharan Africa.
SCD predominantly affects people of African descent but it can also occur in other people, including those of Hispanic, Middle Eastern, Asian and Mediterranean backgrounds. It is more common in these groups because the inherited trait associated with the disease provides protection against malaria, which thrives in warmer climates.
Systemic racism, however, has left patients with fewer experts, lower-quality care, less funding for research, and lower levels of insurance coverage.3 Many people with the disease experience not only physical symptoms but also emotional, social, educational and occupational challenges that quality care could potentially reduce.
Health equity is at the center of the Novartis purpose to improve and extend lives everywhere. In addition to discovering and developing innovative medicines, it is necessary to get these medicines and quality care into the hands of people who need them. This work requires creative ideas and a shared commitment to work together with health systems, governments, patients, and others to improve the reach of quality care and advanced medicines.
When all of us collectively come together and see the challenges, then we can make meaningful change.
Vikki Walton
“Medicines are only one piece of the solution,” says Indranil Bagchi, who leads a Novartis team focused on expanding the reach of medicines to patients with cancer and blood diseases. “That comprehensive holistic picture is missing and that's what we need to work on.”
Nothing to worry about?
Curtis’ personal SCD story started seven years before she was born, with the birth of her older sister. Doctors discovered that Curtis’ sister was a carrier of sickle cell trait, meaning she had one copy of an SCD genetic mutation.
Genes come in pairs, though, and the other gene coding for red blood cells was not mutated, making it unlikely (but not impossible) for her to have sickle cell symptoms. The doctors told the new parents, who each carried the trait but didn’t know it, not to worry.

“Education is so critical, for the patient, for the health provider. It’s needed all around,” says Curtis.
Seven years later, when Curtis was born, her parents were surprised to learn she had SCD – even though the chances are one in four when both parents carry a trait. They learned that her red blood cells would form into the shape of a sickle, or crescent moon, potentially resulting in a blood disorder called anemia. Her blood cells and vessels would also become sticky, making them prone to sometimes clump up and cause episodes of severe and sudden pain, called pain crises, which can lead to organ damage and other complications.
“We have to educate people,” echoes Jincy Paulose, US medical director for sickle cell disease at Novartis.

“We hope these tools help patients communicate better with doctors and help doctors better understand what’s happening to patients,” says Paulose.
Elusive experts
As a child, Curtis received quality care at a hospital that had a special SCD center for children. She learned to advocate for herself. She also learned that staying hydrated, getting rest, avoiding infections and eating healthy food would go a long way toward keeping her well.
Many children in the US have access to supportive sickle cell care. As a result, more people with SCD are surviving into and through adulthood.4 (In contrast, in sub-Saharan Africa, more than half of children born with SCD die before their fifth birthday due to preventable complications. Learn more about our work there.)
Care for adults in the US, however, has not kept pace due in part to a lack of doctors for adult patients. A disproportionately larger number of patients with SCD in the US die between ages 20 and 25. This is also when patients may be unable to find adult care.

“This is where we see the gaps,” says Paulose. “We need to increase the number of adult hematologists that will actually see patients with sickle cell and actually be those experts.”
Curtis experienced this kind of gap when she first had eye trouble. She tried to find a hematologist, a specialist in blood disorders, to help guide and coordinate her care. One particular hematologist with SCD expertise came highly recommended, but getting an appointment was impossible.
So Curtis tracked the doctor down and, medical records in hand, approached her in person at a sickle cell event and asked to become a patient. It worked.
That doctor’s guidance may have saved Curtis’ vision. She referred Curtis to a retina specialist with knowledge of SCD for an immediate re-evaluation.
The shortage of SCD experts came into sharp focus at Novartis about five years ago. “We realized, wow, we are working on potential therapies for patients with sickle cell disease, but there are so many barriers limiting their access to quality care,” says Vikki Walton, a director of state public policy and external affairs at Novartis.
Walton and her colleagues have been working with people living with SCD, physicians and advocacy groups and with policymakers in the US to help address the challenges that patients face in receiving care. Their collective efforts have helped to improve education and awareness of the disease, identify solutions for patients, and increase SCD funding in several states to help address patient needs.
“Everyone has to be a part of this process,” says Walton. “When all of us collectively come together and see the challenges, then we can make meaningful change.”
Day-to-day reality
Curtis has experienced fewer than a dozen pain crises in her lifetime and has been hospitalized only a few times, including once, as a teen, when her spleen urgently needed to be removed.
Yet SCD is a constant part of her life.

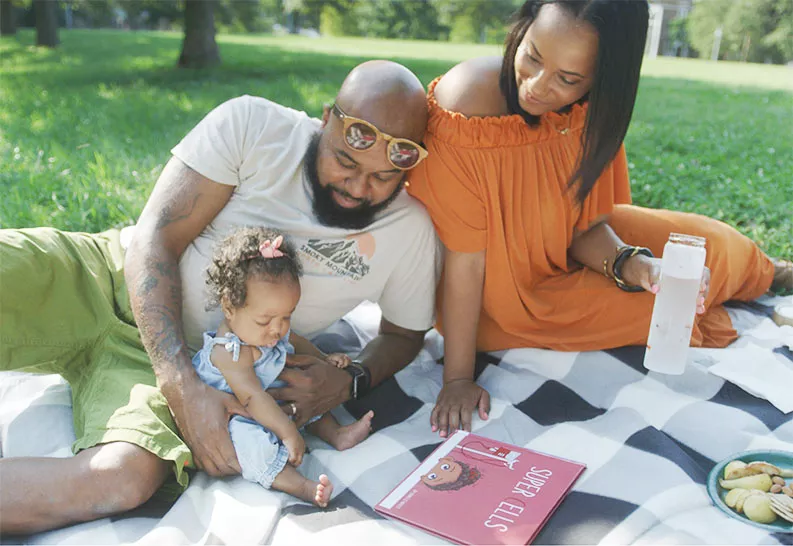
She travels frequently and always asks herself, “What if something happens? Where is the nearest emergency room?” She also had to think carefully when choosing a hospital to deliver her baby. She opted for one with coordinated SCD care located 45 minutes from her home.
It seemed far away, until a doctor pointed out that many people with SCD face steeper challenges. “He said, ‘You have access to the best care you can get, and it's only 45 minutes away.’ He was absolutely right,” says Curtis.
In the US, people with SCD end up in the emergency room or hospitalized far more often than people without the disease. Their medical costs also tend to be far higher. The estimated lifetime cost of care for an SCD patient who lives to age 50 ranges from USD 500 000 to USD 8 million.5
When patients go to an emergency department, for instance during a pain crisis, doctors often treat them as if they were drug seekers rather than patients with a debilitating and painful inherited condition. These kinds of experiences have the potential to perpetuate the mistrust many African Americans have for healthcare systems. (Learn more about our work to build trust.)
Paulose and her team see this challenge as an opportunity. They have worked with emergency room doctors in New York City to help create consensus guidelines for helping patients with SCD.6
“Sometimes that’s the only physician the patient is going to see,” says Paulose. “What if emergency physicians could have a conversation that helps that patient get the care they need?”
There is no one solution to improving care for people with SCD. Progress requires efforts small and large on many fronts.
“We all want quick solutions, but you have to do this kind of work step by step over years,” says Walton. “And it’s not done just by Novartis or industry. It's not just advocacy groups or passionate physicians. It has to be a collective effort.”



